The Addiction Psychiatry Fellowship Program has a great depth and breadth of options for clinical rotations. Clinical rotations are available at a number of sites. Fellows complete about three months of inpatient work and 9 months of outpatient work. See below for details of each rotation and an overview of the 12-month block schedule.
The VA acute care service is a unique service which provides both inpatient care to patients experiencing withdrawal from substances on the inpatient psychiatry floor and consultation services for patients experiencing substance use disorders currently admitted to medical and surgical services. On this educational service, fellows will have the opportunity to work closely with general psychiatry residents, internal medicine residents, and medical students while being supervised provided by an addiction psychiatry attending. See below for specific objectives.
Consultation
- Perform comprehensive evaluations of patients with complex substance use, psychiatric, and medical problems.
- Provide brief interventions and engagement services for individuals experiencing substance use disorders. To learn motivational interviewing, harm reduction techniques, and brief interventions, residents will be supervised on these techniques from an addiction psychiatrist and practice these techniques under supervision.
- Assess and triage appropriate outpatient follow up recommendations in addiction treatment, general mental health, primary care services, or community services.
- Communicate their findings to referring providers, by writing cogent consultation notes that address the pertinent issues and verbally communicate recommendations back to the primary team directly.
Inpatient
- To develop diagnostic acumen residents will, under faculty supervision, perform psychiatric evaluations (and oversee the medical evaluations) including written assessment with multiaxial diagnosis of patients admitted to the inpatient psychiatry unit for detoxification.
- To learn medically supervised withdrawal (detoxification) techniques residents will manage, under faculty supervision, withdrawal of all patients who require it; 2-4 patients per week scheduled.
- To learn to create comprehensive treatment plans, residents will participate in multidisciplinary treatment planning for all patients assigned to their care..
- To learn psychopharmacology for patients experiencing substance use disorders, residents will prescribe appropriate medications for substance use disorders and other psychiatric disorders and manage patients on these medications during their inpatient stays.
- To learn teaching skills residents will participate in teaching and supervision of medical students and general psychiatry residents rotating through the inpatient and consultation service.
The clinic has over 1000 patients experiencing substance use disorders receiving medication assisted treatment. Most patients have co-occurring psychiatric disorders and multiple medical disorders. Residents evaluate new patients, order medications, provide adjunctive psychiatric care, work with nurse practitioners and physician assistants to provide medical care, and attend treatment team meetings. Psychology interns as well as psychology, social work, nursing, and occupational therapy fellows also rotate through the clinic.
Women’s Addiction Treatment
This program treats women only in a gender specific program. Treatment approaches include medication management, group therapy and individual therapy/case management. Residents will treat veterans with primary addiction issues although most women will also have another psychiatric disorder in addition to substance use disorders. Residents can provide psychopharmacologic, individual, and group psychotherapeutic treatment to women Veterans.
VA Intensive Program (10-33% time for 3-9 months)
- To develop diagnostic acumen residents will, under faculty supervision, perform psychiatric and medical evaluations including written assessment with multiaxial diagnosis of an average of one newly admitted patient per week.
- To learn to create comprehensive treatment plans for outpatients and to learn to conduct ongoing individual outpatient treatment, residents will serve as primary individual therapist for one to three active intensive outpatients and develop treatment plans for these patients.
- To learn to utilize multidisciplinary team members, residents will serve as Assistant Medical Director, under faculty supervision, and will direct and manage the team treatment planning and implementation process.
- To learn group therapy techniques residents will be able to co-lead, observe and participate in supervision of support, psychoeducational, process, relapse prevention and introduction to 12-step groups.
- To learn psychopharmacology for patients with substance use disorders, residents will prescribe appropriate medications for SUDs and other psychiatric disorders and manage patients on these medications during their intensive outpatient participation. Specifically residents will learn to perform naloxone challenge tests on patients with opioid use disorder requesting naltrexone therapy. Residents will prescribe naltrexone and follow these patients over time on their medication. Residents will also prescribe disulfiram, acamprosate, and naltrexone for patients with alcohol use disorder and learn how to monitor these patients over the course of their treatment.
- To learn teaching skills residents will participate in the teaching and supervision of general psychiatry residents rotating through the outpatient service.
VA Opioid Treatment Program (10-33% time for 3-9 months)
- To learn about evaluation of opioid use disorder and use of medical treatments, residents will, under faculty supervision, perform psychiatric and medical evaluations including written assessment with multiaxial diagnosis of an average of one newly admitted patient with OUD per week. They will follow these patients over time for appropriate adjustment of buprenorphine or methadone doses.
- To learn to create comprehensive treatment plans for outpatients and to learn to conduct ongoing individual outpatient treatment, residents will serve as primary individual therapist for one to three patients with OUD and develop treatment plans for these patients.
- To learn to utilize multidisciplinary team members, residents will serve as Assistant Medical Director, under faculty supervision, and will direct and manage the team treatment planning and implementation process in the Opioid treatment program.
The Adolescent Substance Abuse Program is located at Seattle Children’s Hospital, the premier pediatric hospital in the five state region. Fellows will evaluate and manage adolescents with psychoactive substance dependence and co-occurring psychiatric disorders in the hospital’s inpatient and emergency room setting. Seattle Children’s Hospital serves many adolescents of both sexes with a wide range of ethnic and racial backgrounds and a wide spectrum of socioeconomic backgrounds. Fellows work closely with the child and adolescent psychiatry attending.
- To learn to evaluate children and adolescents with substance use disorders.
- To learn treatments specific to children and adolescents with substance use disorders.
- To learn family management approaches for families of children and adolescents with substance use disorders.
This program provides consultation to patients experiencing substance use disorders who are hospitalized on medical or surgical units in Harborview. Fellows will learn and practice fundamentals of motivational interviewing, evaluation of substance use disorders, and treatment planning on a multidisciplinary team which include Addiction medicine fellows, psychiatry residents, and medicine residents. The service is supervised by addiction psychiatry and addiction medicine attendings.
- To develop diagnostic acumen residents will, under faculty supervision, perform psychiatric and medical evaluations including written assessment with multiaxial diagnosis of patients.
- To learn motivational interviewing and brief interventions, residents will observe supervisor performing these modalities and then deliver these modalities under supervision.
- To learn to communicate their findings to referring providers, residents will write cogent consultation notes that address the pertinent issues.
- To develop diagnostic acumen in the care of patients experiencing both substance use disorders and cancer, under faculty supervision, residents will perform psychiatric and medical evaluations including written assessment with multiaxial diagnosis of patients.
- To learn to work in interdisciplinary treatment setting, residents will communicate addiction psychiatry assessments and coordinate treatment planning with oncologists, surgeons, radiologists, primary care physicians, and social workers.
This rotation takes place on Tuesday afternoons from 1-5pm. The clinic will be supervised by Mark Duncan MD, and see patients from the University of Washington Northgate primary care clinic. The addiction fellows will provide initial assessment and treatment recommendations across the spectrum of substances and severity of use. It will have a focus on assessing patients for appropriateness for treatment within a primary care setting and provide opportunities for brief follow-up as indicated before returning them to their primary care provider. The rotation will also help the fellow develop expertise in the Collaborative Care model https://www.psychiatry.org/psychiatrists/practice/professional-interests/integrated-care/learn) for integrated mental health treatment, and competency as the psychiatric consultant, within this model. The fellow will learn about the 5 principle of integrated care with a specific focus on the use of a registry and measurement based care, and how to apply those 5 principles of care to integrated treatment efforts for substance use disorders in primary care settings. The clinic will also provide an interdisciplinary training experience for the addiction psychiatry fellows by working alongside and teaching, family medicine residents, integrated care psychology interns, and integrated care psychiatry fellows.
Thursday Schedule (July-June)
8am-12pm: Scholarly Time
Every Thursday is blocked for scholarly activity. Mornings 8-12 are reserved for fellows to work on QI projects, educational presentations, and other scholarly endeavors.
12-1:30pm: University of Washington Psychiatry and Addiction Case Conference Rotation (PACC)
The University of Washington Psychiatry and Addiction Case Conference (UW PACC http://ictp.uw.edu/programs/uw-pacc) is an Extension for Community Health Outcomes (ECHO) based program whose goal is to increase patient access across the state of Washington to effective and evidence based psychiatric and addiction care. UW PACC aims at increasing the knowledge and self-efficacy of all interested health providers within an intentionally supportive virtual community. Fellows will participate in this weekly didactic and case presentation program through a web-based platform from the VA. Other goals of this experience include the development of an appreciation for the challenges urban and rural community providers face in managing psychiatric and addiction patients. Fellows will develop the ability to collaborate with providers in different disciplines and practice settings, around their area of expertise of addiction psychiatry. Activities during the rotation will include the following:
- Participate in each week’s discussion
- Present two clinical cases during a PACC session over the course of the year
- Develop and present 2 didactic talks over the course of the year
- Take on one of 3 roles during the PACC session: Chat Moderator, Expert Panelist for the Day, and Case Recommendation Writer
2-4pm: Didactics/Seminars
4-5pm: Motivational Interviewing Practice
Block Diagram
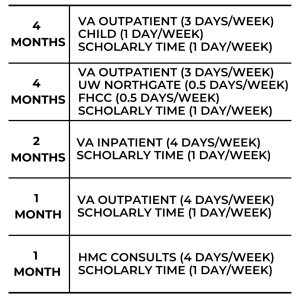
The year is split into 5 blocks. Here is a breakdown of what you would be doing each block.